Plonger dans l’univers des furcations : options thérapeutiques
Conférencier : Nathalie Leow (Royaume Uni) - Responsable scientifique : Guillaume Campard
Dossier ADF 2024, Séances choisies par la team AONEws - AO #72 Février 2025
Les lésions de la furcation (lésions inter-radiculaires) chez le patient atteint de parodontite représentent un défi thérapeutique complexe à relever pour les praticiens. La compréhension de l’anatomie et des stratégies thérapeutiques sont nécessaires pour obtenir un résultat de traitement optimal.
Cette conférence va révéler en quoi une bonne analyse de l’anatomie des atteintes de furcations est importante, rappeler les classifications actuelles et évoquer les modalités pour établir un diagnostic précis. A l’aide d’une revue exhaustive des options thérapeutiques scientifiquement démontrées, incluant des techniques conventionnelles ou plus contemporaines telles que les thérapeutiques non chirurgicales, la chirurgie résective ou régénérative, les participants ont pu avoir un aperçu global des traitements des atteintes de furcation. De plus, cette présentation a traité du concept de soins centrés sur le patient, en mettant l’accent sur le rôle de la communication et de la prise de décision concertée, afin d’obtenir le succès thérapeutique. En combinant les données cliniques et bibliographiques, cette présentation a fourni aux praticiens les connaissances nécessaires pour relever le défi des atteintes de furcation, améliorer leur pratique clinique et promouvoir la santé parodontale de leurs patients à long terme.
La conférence a été donnée en anglais, ainsi, afin de respecter l’exactitude des propos de la conférencière, j’ai choisi de vous présenter le résumé en anglais.
The lecturer, Dr Nathalie Leow, who is a Clinical Associate Professor in Periodontology at UCL Eastman Dental Institute and the Deputy Programme Director of the MClinDent in Periodontology, didn’t allow to take pictures of her lecture.
Introduction
Furcation lesions in patients with periodontitis represent a complex challenge for dental practitioners. These lesions necessitate a thorough understanding of molar anatomy, precise diagnostic techniques, and evidence-based therapeutic strategies to ensure successful outcomes. This report explores the multifaceted nature of furcation lesions, focusing on classification, treatment modalities, and the integration of patient-centered care to achieve optimal periodontal health.
Complex anatomy of furcation lesions
A detailed understanding of furcation anatomy is crucial in assessing the healing potential of affected sites. Key anatomical features influencing prognosis include :
- Root Trunk Length: shorter root trunks generally exhibit better outcomes due to more accessible treatment areas to personal and professional thorough cleaning;
- Root Divergence: the separation of roots affects the feasibility of cleaning and surgical interventions. Divergent roots are often more favorable to better treatment outcomes.
- Specific Anatomical Variations: pits, fissures, and grooves on molars complicate cleaning and increase susceptibility to biofilm accumulation. Sometimes, root management such as root planning can be practiced.
These factors underscore the need for personalized treatment planning.
Classification and diagnostic modalities
Accurate classification and diagnosis are foundational for effective management.
- Hamp Classification: the horizontal classification, a clinical measure thanks to a curved Nabor’s probe. Grade I: Minimal horizontal bone loss <3mm, often undetectable on radiographs. Grade II: Partial horizontal loss between 3 and 6mm, visible radiographically. Grade III: Through-and-through bone loss, the most severe type > 9mm.
- Tarnow Classification : focuses on vertical bone loss and its severity.
- Diagnostic tools:
Clinical probing with curved furcation probes (e.g., Nabor’s probe).
Radiographic imaging: two-dimensional (2D) radiographs for general assessment and cone-beam computed tomography (CBCT) for detailed, three-dimensional (3D) evaluation. Dr Leow always does a CBCT before surgery to plan very precisely her treatment.
Prognosis: Grade II and III furcations are associated with poorer long-term outcomes, highlighting the importance of early detection.
Treatment modalities
Management of furcation lesions involves both non-surgical and surgical approaches, tailored to the lesion's severity and patient-specific factors.
Non-surgical therapy
- Initial therapy goals: disruption of the biofilm and removal of deposits.
- Techniques: ultrasonic tips designed for furcation areas are more effective than traditional curettes.
- Limitations: non-surgical methods alone are insufficient for treating advanced (Grade II and III) lesions.
When non-surgical methods are inadequate, surgical interventions become necessary.
- Resective Surgery: Removal of dental tissue or bone to improve access and reduce lesion severity.
- Access Flap or Open Flap Debridement (OFD) : Indicated for persistent deep probing depths (>5mm) and bleeding. Requires excellent patient compliance and oral hygiene.
- Root resection and separation : Suitable for teeth with substantial bone loss around one root but good support around others. Indications include persistent probing depths, strategic tooth value, and favorable root divergence.
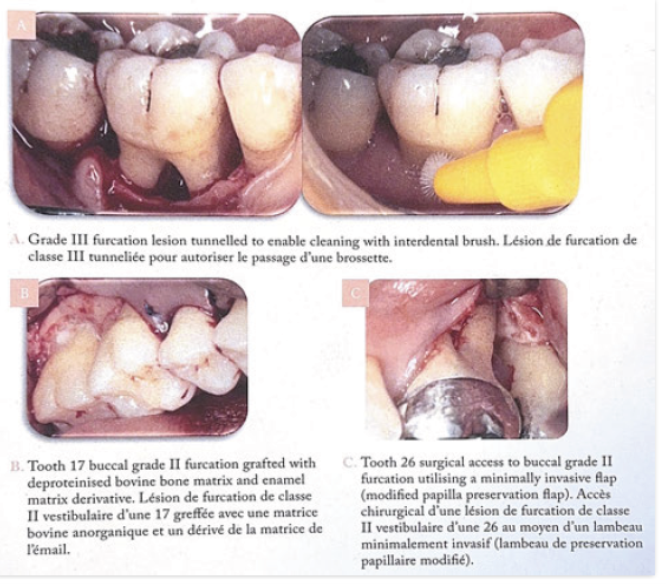
- Tunneling surgery : Effective for Grade II or III furcations with two or more entrances. Requires patient dexterity and optimal oral hygien
Regenerative therapy
- Targets Grade II lesions with adequate bone support and controlled risk factors (e.g., diabetes, smoking).
- Surgical regeneration involves advanced techniques and operator expertise. Favorable tooth characteristics, such as short root trunks, are critical for success.
Long-term maintenance
Ongoing periodontal maintenance is essential for sustaining periodontal health and minimizing recurrence. Regular follow-ups, professional cleaning, and patient education about oral hygiene practices form the cornerstone of effective maintenance protocols.
Future perspectives
Advancements in technology, particularly artificial intelligence (AI), promise to transform the management of furcation lesions:
- Early Diagnosis and Detection: AI-le tripowered tools can identify lesions earlier and more accurately.
- Predictive Analytics: AI may help forecast disease progression and tailor treatment plans.
- Patient Education: Personalized, data-driven insights can enhance communication and compliance.
Conclusion
Addressing furcation lesions requires an integrative approach that combines clinical expertise, cutting-edge technology, and patient-centered care. By understanding lesion anatomy, leveraging precise diagnostic tools, and applying tailored therapeutic strategies, practitioners can overcome the challenges posed by these complex cases and promote long-term periodontal health.
This comprehensive review equips dental professionals with the knowledge and tools to navigate the intricacies of managing furcation lesions, ultimately improving patient outcomes and enhancing their clinical practice.
Ce qu’il faut retenir :
Le traitement des lésions de furcation molaires de classe II et III avec poches résiduelles doit bénéficier autant que possible d’un traitement parodontal avancé.
Le maintien, le traitement et la maintenance de dents avec des atteintes de furcation restent la solution la moins coûteuse pour le patient par rapport à l’extraction et le remplacement par des prothèses implanto-portées.
